Veterinary college researchers work to protect people from deadly effects of nerve gases
A veterinary pharmaco-toxicologist in the Virginia-Maryland Regional College of Veterinary Medicine at Virginia Tech is leading a team that has been awarded almost $1 million from the National Institutes of Health to explore the development of a nanotechnology-based approach for protecting people from the deadly effects of nerve gases like Sarin, VX, and others that can be used as agents of terror.
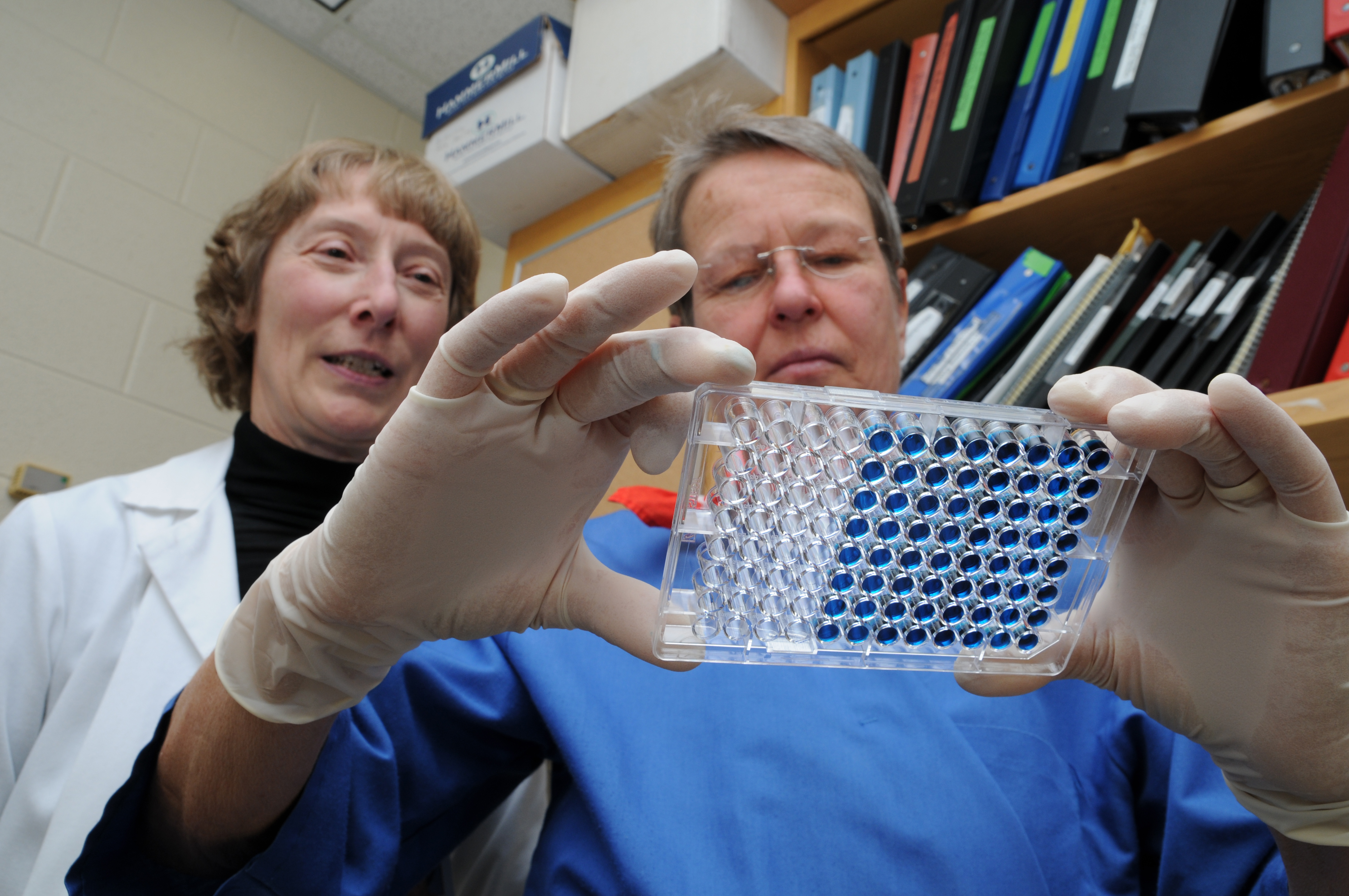
Marion Ehrich, a professor in the Department of Biomedical Sciences and Pathobiology and co-director of the Laboratory for Neurotoxicity Studies, will spend three years developing novel methods for delivering chemical antidotes that can mitigate the devastating effect of organophosphate-based neurotoxicants.
The experiments will involve the use of nanoparticles called fullerenes -- commonly known as “Buckyballs” -- that have been modified to enhance their water solubility and catalytic and antioxidant properties. The nanoWorks and Biomedical Technologies Group of Luna Innovations Inc. of Roanoke, Va., the company that is partnering with Ehrich on the work, are developing the fullerene derivatives and supporting immunoreagents.
“Organophosphorous compounds represent a class of extremely potent chemical warfare agents that can cause incapacitation and death within minutes of exposure,” said Ehrich. The 1994 and 1995 Japanese subway attacks conducted by terrorists using sarin gas and the attacks on the northern Iraqi Kurds perpetrated by former dictator Saddam Hussein are both examples of chemical terrorism and warfare using organophosphate compounds, according to Ehrich.
These agents work by inhibiting the production of the enzyme acetylcholinesterase, which metabolizes the neurotransmitter acetylcholine, an agent that plays a critical role in movement and other physiological processes like respiration and digestion.
The resulting proliferation of the neurotransmitter acetylcholine unleashes a cascading sequence of clinical problems, including salivation, lacrimation or tearing of the eyes, urination, defecation, tremors, seizures, and eventually paralysis as the wildly firing synaptic junctions eventually cause muscle exhaustion, paralysis, and death.
The conventional therapeutic approach for treating nerve gas exposure is to administer atropine, which blocks cholinergic receptors, and pralidoxime or 2-PAM, which can remove the organophosphate compounds from the acetylcholinesterase, explains Ehrich, provided it is administered in time.
But there are inherent limitations on the effectiveness of atropine against nerve gases that depend largely upon the amount of the agent the victim is exposed to and the amount of time that passes between the toxic insult and the time that the atropine is administered. Also, while the atropine can be effective in dealing with what is commonly referred to as the SLUD effects (salivation, lacrimation, urination, and defecation), it is not effective in dealing with the brain damage that is caused by oxidative stress, or the tissue-destroying oxygen-free radicals that are generated by the toxicants.
This is because the atropine cannot pass through the “blood-brain barrier,” a vascular network of brain capillaries with dense intercellular junctions that combine to create a biologically protective “sheathe” that permits some molecules to pass but inhibits others.
The inability of the atropine to pass through the blood-brain barrier substantially limits the ability to prevent the critical neurologic threat caused by the uncontrolled seizures, and the secondary neurological damage that is caused by the oxygen free-radicals generated following the seizures.
“The water-soluble fullerenes developed by Luna Innovations are an absolutely critical part of this novel approach to developing better counter-measures,” said Ehrich. “We’re delighted to be collaborating with them.” Luna Innovations engages in the research, development, and commercialization of technologies in the areas of test measurements, sensing instrumentation, and health care.
Ehrich hopes the research will be effective in two ways. First, and most important, she has preliminary results that suggest the fullerene derivatives will bind with the free organophosphate compounds. This would protect the body because the toxicants have not yet begun to exert their toxic affect.
“I want something that is going to scavenge the organophosphates,” said Ehrich, who is a past president of the 6300-member national Society of Toxicology, underscoring the importance of developing countermeasures that are more effective than just atropine.
Second, since the fullerenes should be effective in crossing the blood brain barrier, she believes they should be effective in mitigating the oxygen free-radicals that play a role in the development of seizures.
The National Institutes of Health R21 grant provides $946,432 in funding, including the Luna Innovations sub-contract. It is expected to support a three-year research effort. The researchers hope to identify two effective fullerenes by May 2009 using in vitro experiments, and focus future study on those.




